Navigating a Looming Crisis: How Policy Changes Threaten Affordable Healthcare Access Through the ACA Marketplaces
The Affordable care Act (ACA) Marketplaces have dramatically expanded health insurance coverage in the United States. Though, a confluence of impending policy changes and proposed alternatives to current subsidies threaten to unravel these gains, possibly pushing millions back into the ranks of the uninsured. As key provisions are set to expire or be altered, a recent survey of leading health policy experts paints a concerning picture, revealing a significant disconnect between legislative intentions and the likely real-world consequences for affordability and access. this article delves into these critical issues, providing a thorough analysis of the challenges ahead and their potential impact on american healthcare.
The Context: Expiring subsidies and the Search for alternatives
Currently, enhanced Premium Tax Credits (ePTCs) are instrumental in making marketplace coverage affordable for millions. Though,these credits are scheduled to expire at the end of 2025,creating a policy vacuum that demands immediate attention. Policymakers are actively exploring alternatives, but emerging proposals are facing strong criticism from the very experts whose insights are crucial to informed decision-making. The core issue isn’t simply about cost; it’s about ensuring continued access to coverage for those who rely on the Marketplace.
The HSA pivot: A Well-Intentioned But Flawed Solution?
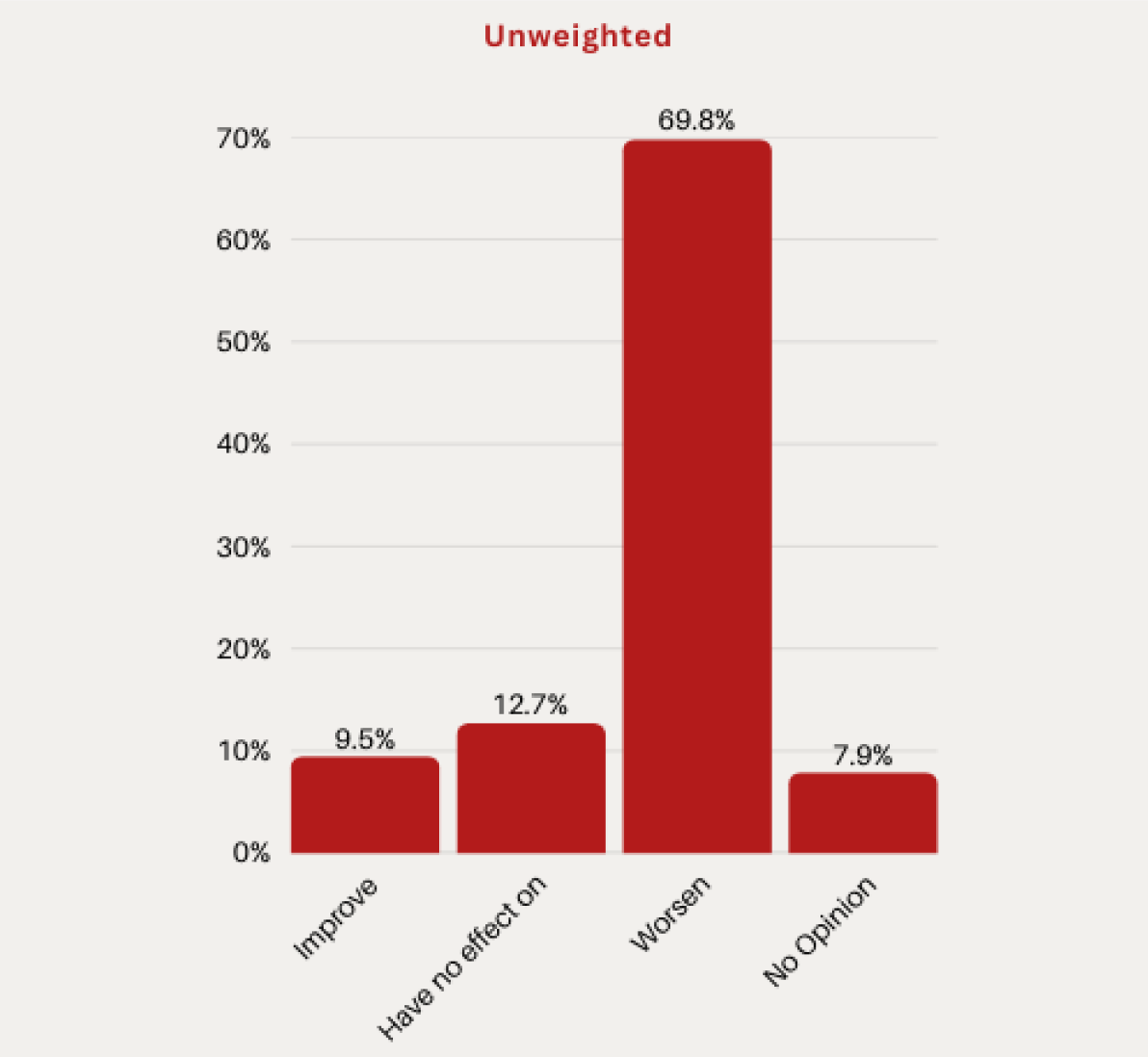
One prominent proposal, championed by Senator Bill Cassidy (R-LA), suggests depositing the value of ePTCs into Health Savings Accounts (HSAs) instead of applying them directly to monthly premiums. The rationale is to empower consumers wiht greater control over their healthcare spending. Though,a resounding 70% of surveyed scholars believe this shift would “measurably worsen” affordability for Marketplace enrollees,with only 10% anticipating an enhancement.
This negative assessment stems from a basic flaw: decoupling the subsidy from the premium creates significant cash-flow challenges for lower-income individuals. Requiring upfront payment of the full premium before accessing HSA funds presents a considerable barrier to entry, potentially leading to disenrollment and delayed care. HSAs are most beneficial for those with consistent income and the ability to plan for healthcare expenses – characteristics not universally shared by Marketplace enrollees. This approach risks exacerbating existing health inequities.
The Illusion of ”Skin in the Game”: The Risks of Small-Dollar Premiums
Another debated policy centers on the prevalence of “zero-dollar” premium plans, made possible by the enhanced subsidies. Concerns about potential fraud and passive enrollment have led some to propose a mandatory “token” premium of $5 to $10 per month. While proponents argue this fosters “skin in the game,” the expert consensus suggests the downsides far outweigh the benefits.
A striking 75% of experts agree that even a nominal premium would reduce enrollment among eligible individuals who intend to remain covered. While 70% believe it would reduce the number of unaware enrollees, only 37% anticipate a measurable reduction in fraudulent enrollment.The data clearly indicates that even a small financial hurdle introduces administrative friction – failed payments, expired credit cards, and lost mail – that disproportionately impacts those who need coverage the most. This seemingly minor change could trigger a significant loss of coverage.
The Silent Threat: The End of Automatic Re-Enrollment and the Burden of Administrative Tasks
Perhaps the most concerning development is a policy already enshrined in law: the elimination of passive (automatic) re-enrollment, slated for 2028 under the “One Big Lovely Bill Act” (HR 1). Currently, enrollees who take no action are automatically re-enrolled with their subsidy intact. This streamlined process is a critical safeguard against coverage gaps.
The new law requires enrollees to actively re-verify their income and eligibility annually. The expert response to this change was overwhelmingly negative: a staggering 81% of respondents agreed or strongly agreed that eliminating passive re-enrollment will “substantially reduce” Marketplace enrollment. This finding aligns with established research on “administrative burden,” which consistently demonstrates that increased administrative requirements lead to decreased participation in benefit programs. The implications are clear: adding another layer of complexity will inevitably result in eligible individuals losing their coverage.
Why This Matters: The Broader Implications for Healthcare Access
These proposed and enacted changes aren’t isolated policy decisions; they represent a fundamental shift in the approach to healthcare affordability and access. The expert consensus consistently points to a common theme: policies designed to address perceived inefficiencies or promote individual obligation risk undermining the core goal of the ACA – expanding coverage and improving health outcomes.
the potential consequences are far-reaching:
* increased Uninsured Rates:




![Watch [Show Name] Finale: Stream HBO Max – Date, Time & Options Watch [Show Name] Finale: Stream HBO Max – Date, Time & Options](https://i0.wp.com/media-cldnry.s-nbcnews.com/image/upload/t_social_share_1200x630_center%2Cf_auto%2Cq_auto%3Abest/rockcms/2025-12/hudson-williams-connor-storrie-heated-rivalry-en-122425-ec3773.jpg?resize=150%2C100&ssl=1)



