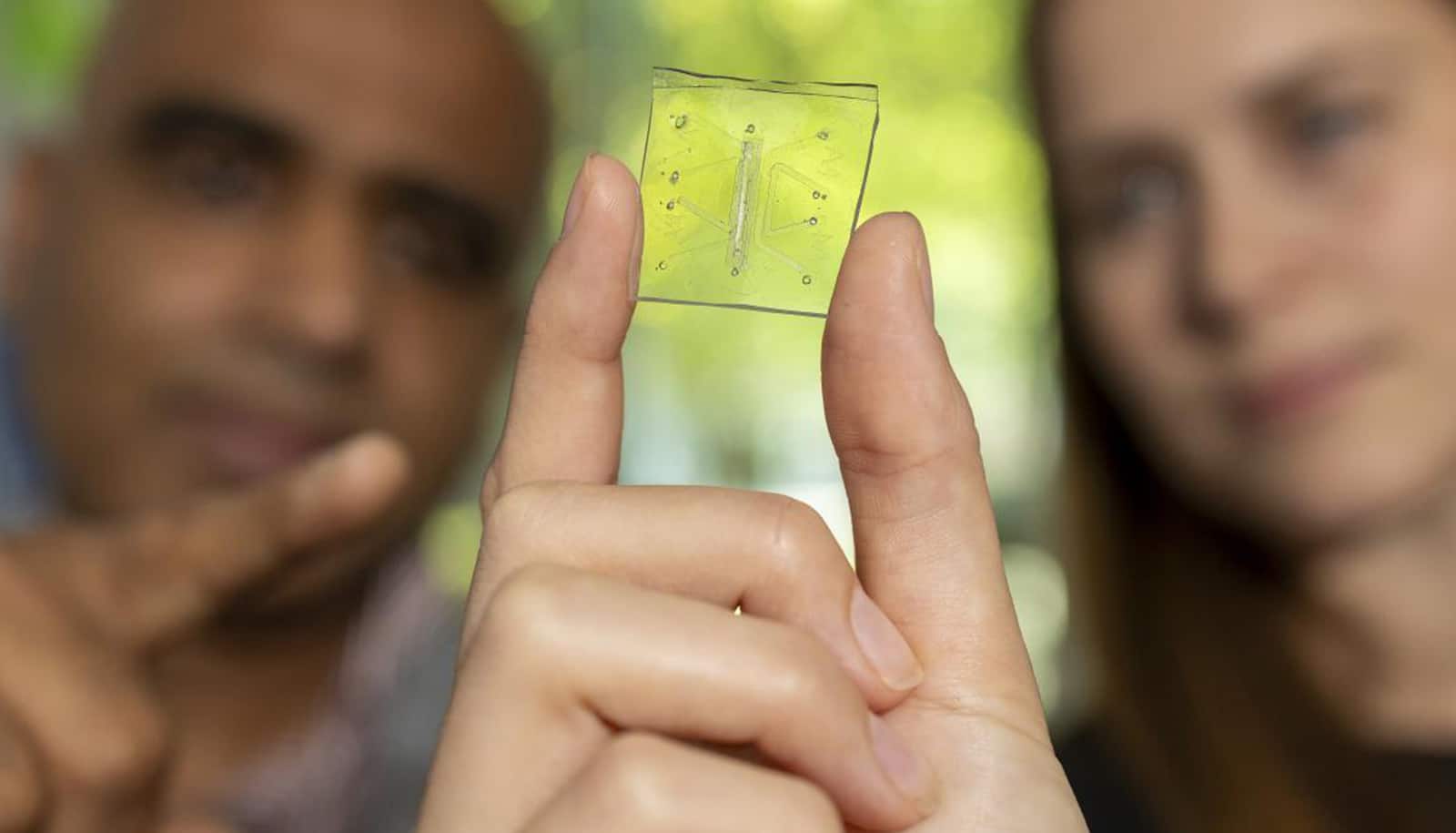
A Revolutionary “Lung-on-a-chip” Mimics Human Immunity, Paving the Way for Personalized Medicine & Reduced Animal Testing
For decades, lung disease research has faced a critical hurdle: accurately replicating the complexities of the human lung in vitro. Traditional methods relying on animal models frequently enough fall short, failing to fully capture the nuances of human immune responses and disease progression. But a groundbreaking development from Georgia Tech researchers is poised to change that – a “lung-on-a-chip” that doesn’t just mimic lung structure, but actively defends itself against infection, mirroring the human body’s own immune response.
This isn’t just a scientific advancement; it’s a potential paradigm shift in how we understand, treat, and even prevent lung diseases. Let’s delve into the details of this remarkable innovation and its implications for your health and the future of medical research.
The Personal Connection: Driven by Loss, Fueled by Innovation
The story behind this breakthrough is deeply personal. Lead researcher Krish Roy’s motivation stems from the loss of his uncle to a lung disease. “If work like this means fewer families lose someone they love,then it’s worth everything,” he explains,highlighting the powerful human drive behind the science.
This dedication, coupled with the expertise of his colleague, Singh, propelled their team to reimagine the possibilities of organ-on-a-chip technology. They weren’t simply aiming to build a model; they were striving to recreate a living, breathing, defending lung.
The breakthrough: Witnessing Immunity in Action
The turning point arrived when the team observed something unprecedented under the microscope. For the first time, they witnessed blood and immune cells flowing through the chip’s tiny vessel-like structures, behaving identically to those within a living human lung.
This was a monumental achievement. Previously, adding immunity to these systems proved incredibly challenging. Immune cells frequently enough perished quickly or failed to interact with the lung tissue effectively. Roy and Singh’s team solved this critical problem, creating an habitat where immune cells could thrive and mount a coordinated defense.
* The Challenge: Maintaining immune cell viability and function within a microfluidic chip.
* The Solution: Developing a chip environment that supports immune cell survival and coordinated response.
* The Result: A functional immune system within the lung-on-a-chip.
Validating the Model: A Realistic Response to infection
to truly test their creation, the researchers introduced a severe influenza virus. The chip’s response was remarkable. It closely mirrored the immune response observed in actual patients:
* Immune cells rapidly migrated to the infection site.
* Inflammation spread through the tissue.
* Defensive mechanisms activated in a coordinated manner.
“That was when we realized this wasn’t just a model,” Singh stated. “it was capturing the real biology of disease.” This validation is crucial, demonstrating the chip’s ability to accurately represent the complexities of human lung function.
Why This Matters: Beyond Animal Models & Towards Personalized Medicine
For years, lung research has heavily relied on animal models. However, these models often fail to accurately reflect human physiology. Mice,such as,don’t experience asthma likewise children do,and their immune systems respond differently.
This new lung-on-a-chip offers a important advantage:
* Increased Accuracy: It can reflect the inherent variability between individuals, something animal models can’t replicate. “Five mice in a cage may respond the same way, but five humans won’t,” singh explains.
* Reduced Animal Testing: The FDA is actively seeking to reduce animal testing, and this technology aligns perfectly with that goal. As Roy emphasizes, the device provides “unprecedented insights into the complex lung immune response.”
* Personalized Medicine Potential: The long-term vision is to create chips using your own cells, allowing doctors to predict which therapies will be most effective for you.
Expanding the Scope: From Influenza to a Wider Range of Diseases
The initial success with influenza is just the beginning. Roy and Singh believe this platform can be adapted to study a wide array of lung diseases,including:
* Asthma
* Cystic Fibrosis
* Lung Cancer
* Tuberculosis
Furthermore,they are actively working to integrate other