Decoding Sepsis: New Insights into Patient Subtypes and Immune Response
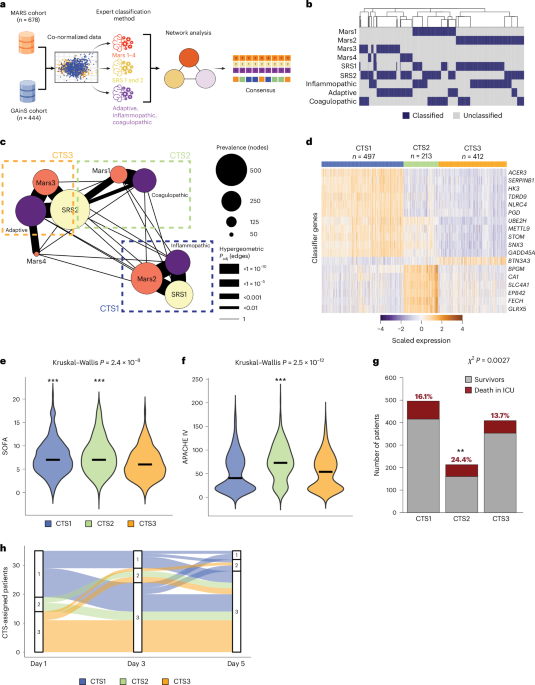
Sepsis, a life-threatening condition arising from the body’s overwhelming response to infection, isn’t a single disease. Recent research reveals distinct subtypes, or clusters, of sepsis – categorized as CTS1, CTS2, and CTS3 – each characterized by unique biological signatures. Understanding these differences is crucial for tailoring treatment and improving patient outcomes.
What are Clinical Trait subtypes (CTS)?
These CTS classifications aren’t based on the initial infection site, but rather on the way your body responds to the infection at a cellular and molecular level. Identifying these subtypes allows for a more precise understanding of the underlying mechanisms driving sepsis in individual patients. Let’s explore what sets each CTS apart.
CTS1: The Inflammatory Response
CTS1 represents the largest group studied, and it’s marked by a robust inflammatory state. Patients in this subtype exhibit heightened levels of inflammatory mediators and increased activity of neutrophils, a type of white blood cell critical for fighting infection.
* specifically, you’ll see elevated levels of molecules involved in inflammation and endothelial function.
* Endothelial barrier integrity - the health of your blood vessel linings – appears compromised in CTS1.
* Interestingly, despite changes in fibrinolysis and anticoagulation, the overall rate of clot formation and breakdown remains consistent.
Essentially, CTS1 signifies a body actively, and intensely, fighting infection, but potentially causing collateral damage thru excessive inflammation.
CTS2: Heme Metabolism and Fibrinolytic Disturbances
CTS2 patients present a different picture. This subtype is characterized by a distinct signature related to heme metabolism – the breakdown of red blood cells.
* You’ll find disturbances in the fibrinolytic system, which is responsible for dissolving blood clots.
* This suggests potential issues with blood clotting and the body’s ability to regulate it effectively.
* Compared to the other subtypes, CTS2 demonstrates unique molecular and cellular alterations.
CTS2 highlights a disruption in crucial physiological processes beyond just the initial inflammatory response.
CTS3: A Milder Presentation
CTS3-classified patients generally exhibit less severe cellular and molecular disturbances.This suggests a less aggressive form of sepsis, potentially indicating a more contained or resolving infection.
* Biomarker levels in CTS3 are generally lower and less dramatically altered compared to CTS1 and CTS2.
* This doesn’t mean CTS3 is harmless, but it suggests a different trajectory and potentially a better prognosis.
putting it All Together: A New Framework for understanding sepsis
These findings are paving the way for a more nuanced understanding of sepsis. The research suggests that each CTS is driven by different cell types and biological pathways.
* CTS1 likely involves immune cells actively battling infection.
* CTS2 appears linked to disruptions in heme metabolism and blood clotting.
* CTS3 represents a less pronounced systemic response.
This new taxonomy, visualized through detailed diagrams, offers a extensive overview of the key features driving each subtype. It’s a significant step toward personalized medicine in sepsis, where treatment strategies can be tailored to your specific subtype for optimal outcomes.
What Dose This Mean for You?
While this research is still evolving, it offers hope for improved sepsis care. By identifying your specific CTS, healthcare professionals can potentially:
* Predict your risk of complications.
* Select the most effective therapies.
* Monitor your response to treatment more accurately.
Ultimately, a deeper understanding of sepsis subtypes will lead to more targeted and effective interventions, saving lives and improving the quality of care for those affected by this devastating condition.