The Evolving Landscape of Medicare Physician Payments: challenges and Potential Reforms
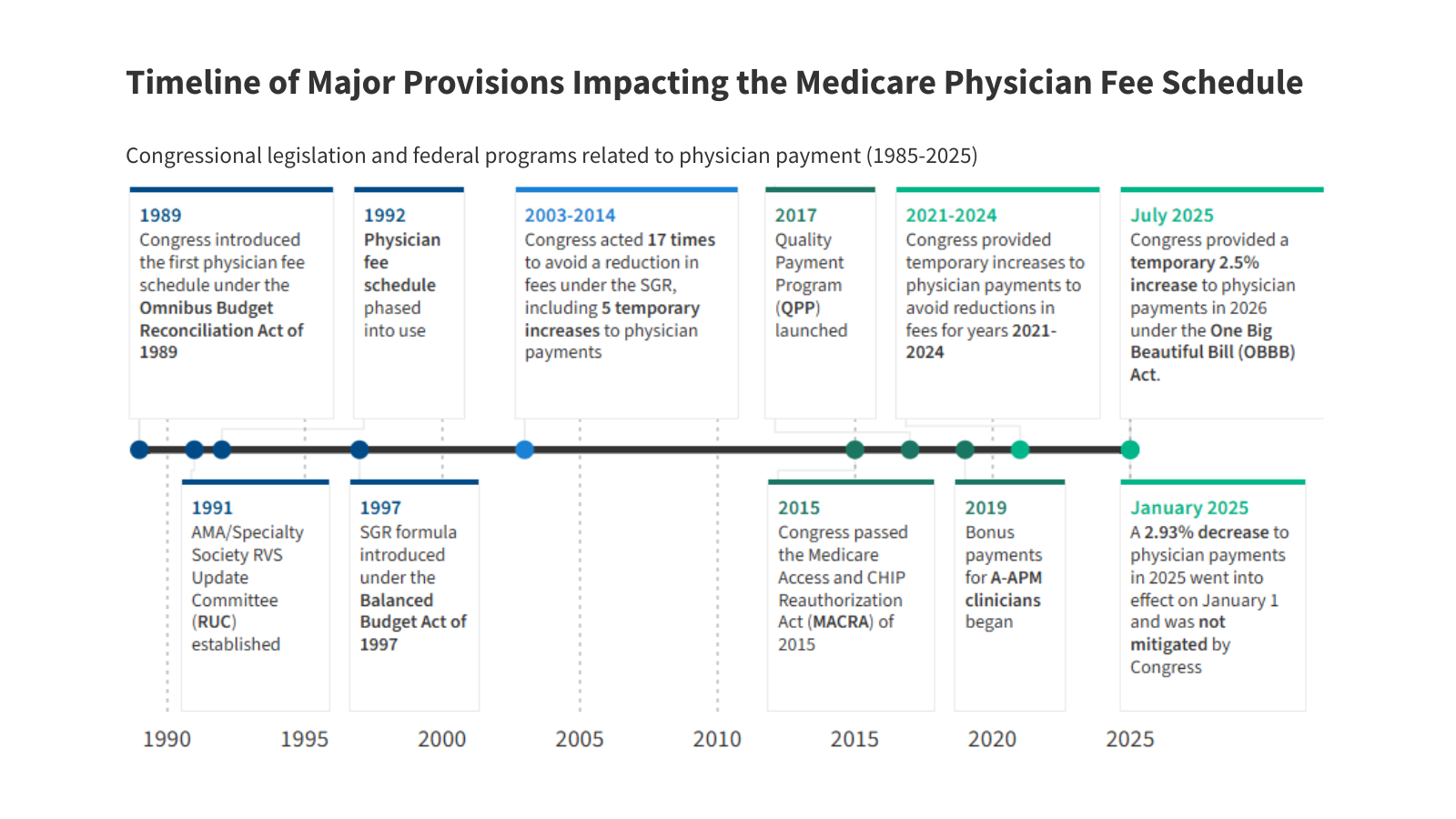
For decades, ensuring fair and sustainable payment for physicians within the Medicare system has been a persistent challenge. Recent activity signals a growing momentum for critically important reform, a decade after the passage of the Medicare Access and CHIP Reauthorization Act (MACRA) - the last major overhaul. This article dives into the complexities of physician payment, current pressures, and emerging strategies being considered by policymakers.
The Current System: A Balancing Act
The existing fee-for-service (FFS) model, while still dominant, faces increasing scrutiny. Maintaining adequate physician compensation while simultaneously controlling escalating healthcare costs is a delicate balancing act. Several factors contribute to this tension:
* Conversion Factor Concerns: The conversion factor, a key component in calculating physician payments, has faced consistent downward pressure. This threatens physician revenue and potentially access to care.
* Budget Neutrality Requirements: policies designed to ensure payment changes don’t increase overall Medicare spending (budget neutrality) can inadvertently lead to cuts in other areas.
* Reliance on the RUC: The Relative Value Update Committee (RUC), a committee of the American Medical Association (AMA), historically plays a significant role in advising CMS on the relative value of medical services. Increasingly, there’s a push for greater independence from this influence.
Shifting Away from Fee-for-Service
Recognizing the limitations of FFS, there’s a growing emphasis on alternative payment models (A-APMs). These models incentivize value-based care, focusing on quality and outcomes rather than volume.
* A-APMs: A Gradual Transition: While A-APMs have shown promise, participation has generally remained limited. The Medicare Payment Advisory commission (MedPAC) proposes a voluntary programme mirroring A-APM structures to encourage a more gradual shift for clinicians.
* MIPS’ Limited Impact: The merit-based Incentive Payment System (MIPS), intended to reward high-performing physicians, has also seen relatively low engagement.
Legislative and Administrative Efforts for Reform
Both Congress and the Centers for Medicare & Medicaid Services (CMS) are actively exploring potential solutions.
* Legislative Proposals: Several bills have been introduced to address payment challenges, including:
* Raising or modifying the budget neutrality threshold.
* offering separate conversion factor updates for primary and specialty care. This would give CMS more versatility in adjusting rates based on policy priorities.
* Senate Finance Committee Focus: The Senate finance committee has held hearings and released a whitepaper outlining options to:
* Stabilize conversion factor updates.
* Extend access to telehealth.
* Incentivize A-APM participation.
* CMS Rulemaking Changes (2026): CMS has proposed changes to how relative value calculations are determined. This includes incorporating data from sources beyond the AMA/RUC, such as the Medicare Hospital Outpatient Prospective Payment System and the Medicare economic Index. This move aligns with HHS Secretary Robert Kennedy Jr.’s goal of reducing reliance on the RUC and fostering internal code review.
What Does This Mean for You?
If your a physician, understanding these changes is crucial. Here’s what you should consider:
* Stay Informed: Keep abreast of proposed rules and legislative developments.CMS and the Senate Finance Committee websites are excellent resources.
* explore A-apms: Evaluate whether participating in an A-APM aligns with your practice goals and capabilities.
* Advocate for Your practice: Engage with professional organizations and policymakers to voice your concerns and contribute to the discussion.
The Road Ahead
The future of Medicare physician payment remains uncertain. Though,the increasing attention to reform signals a recognition that the current system is unsustainable. Designing payment approaches that adequately compensate physicians while controlling costs will require careful consideration and collaboration between policymakers, providers, and stakeholders. Successfully navigating this complex landscape will be essential to ensuring continued access to high-quality healthcare for Medicare beneficiaries.
Disclaimer: This work was supported in part by Arnold Ventures. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
Resources:
* [CMS Alternative Payment Models](https://www.cms.gov/priorities/innovation/key-concepts/alternative-payment-models-apms#:~:text=Alternative%