The Rise of Remote patient Monitoring: A 2025 Deep Dive
The healthcare landscape is undergoing a seismic shift, driven by technological advancements and a growing need for accessible, proactive care. at the forefront of this conversion is remote patient monitoring (RPM), a technology rapidly gaining traction and reshaping how we deliver and receive healthcare. As of November 6th, 2025, the adoption of RPM is accelerating, fueled by recent data indicating a significant increase in insurer claims for these services. A recent KFF and peterson Center on Healthcare analysis reveals an estimated 300,000 adults with employer-sponsored health coverage had at least one RPM claim in 2023 – a number expected to climb substantially in the coming years.This article provides a comprehensive overview of RPM, exploring its benefits, applications, costs, challenges, and future trends.
What is Remote Patient Monitoring?
Remote patient monitoring involves using digital technologies to collect physiological data from patients in their homes and securely transmit that facts to healthcare providers. This data can include vital signs like blood pressure, heart rate, weight, blood glucose levels, and even patient-reported outcomes like pain levels and medication adherence. It’s more than just data collection; it’s about enabling proactive intervention and personalized care plans.
Who Benefits from Remote Patient Monitoring?
While RPM can benefit a wide range of patients, certain demographics and conditions are seeing the most significant impact. Recent trends (late 2024 – early 2025) show a clear pattern:
* Older Adults: Individuals aged 65 and older are disproportionately benefiting from RPM, particularly those managing chronic conditions. This is largely due to the convenience and reduced need for frequent in-person visits.
* Women: Data consistently shows higher RPM utilization among women compared to men, potentially linked to a greater prevalence of chronic conditions like hypertension and a proactive approach to healthcare.
* Chronic Condition Management: RPM is proving particularly effective in managing:
* Hypertension & Circulatory Diseases: Continuous blood pressure monitoring allows for timely adjustments to medication and lifestyle interventions.
* Musculoskeletal Conditions: Tracking activity levels and pain scores helps optimize physical therapy and pain management strategies.
* Diabetes: Remote glucose monitoring empowers patients to better manage their blood sugar levels and prevent complications.
* Heart Failure: Monitoring weight, blood pressure, and heart rate can detect early signs of decompensation, allowing for prompt intervention.
* Chronic Obstructive Pulmonary Disease (COPD): Monitoring oxygen saturation and respiratory rate can help prevent exacerbations.
The Cost of Remote Patient Monitoring: A Breakdown
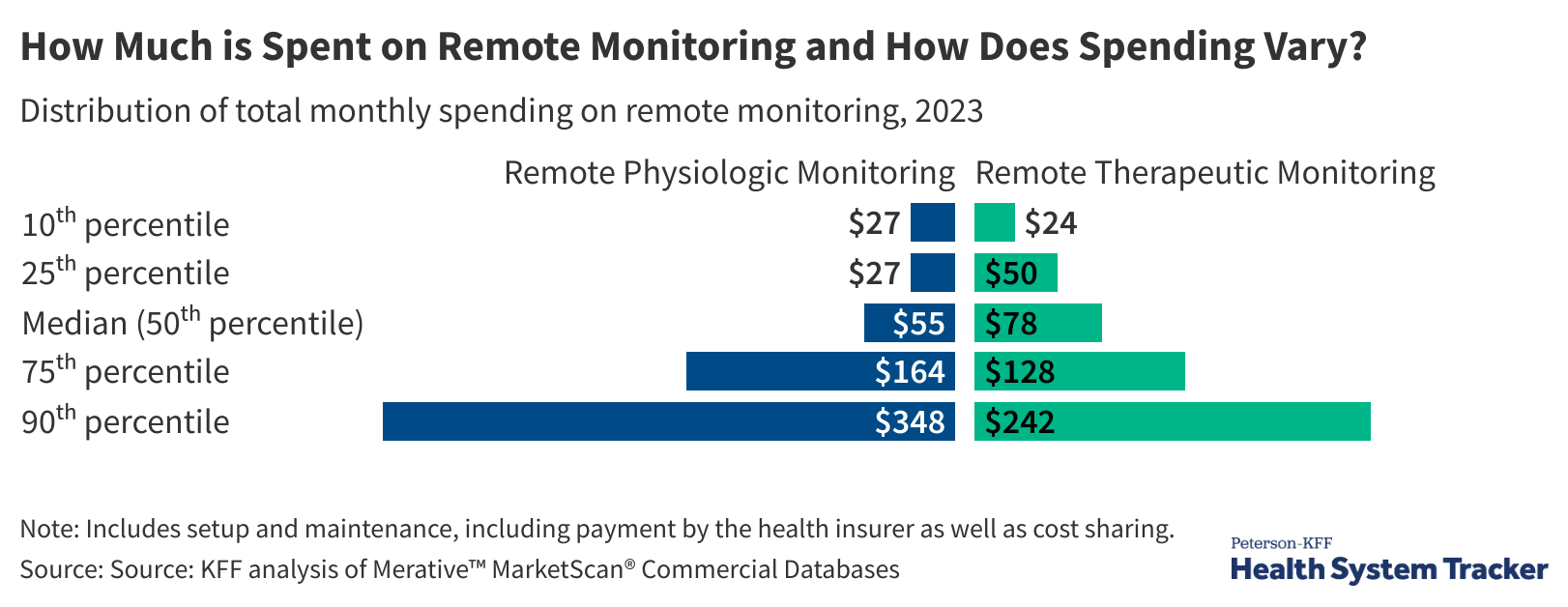
Understanding the financial implications of RPM is crucial for both patients and providers. The KFF analysis highlights the varying costs associated with different types of monitoring:
* Physiological Data Monitoring: The median cost is approximately $55 per month ($12 out-of-pocket), covering the monitoring of physical data like blood pressure and weight.
* Self-Reported Data Monitoring: Monitoring patient-reported outcomes, such as pain levels and medication adherence, averages $78 per month ($21 out-of-pocket).
These costs typically include the device itself, data transmission, and clinical oversight. however, it’s important to consider the potential cost savings associated with RPM, such as reduced hospital readmissions and emergency room visits. A 2024 study published in the Journal of the American Medical Association demonstrated a 20% reduction in hospital readmission rates for heart failure patients enrolled in an RPM program.