Unlocking Cancer Immunotherapy: New Research Reveals the Root of T-Cell Exhaustion
For decades, cancer immunotherapy has held immense promise, harnessing the body’s own immune system to fight tumors. However, a significant hurdle has remained: T-cell exhaustion. These critical immune cells, responsible for recognizing adn destroying cancer cells, often become ineffective, limiting the success of immunotherapy treatments. Now, a groundbreaking study from The Ohio State University Complete cancer Center - Arthur G. James Cancer hospital and Richard J. Solove Research Institute (OSUCCC – James) has identified a previously unknown mechanism driving this exhaustion – a proteotoxic stress response within T-cells – and offers a novel pathway to revitalize these cells and dramatically improve cancer treatment outcomes.
The Puzzle of T-Cell Exhaustion: A long-Standing Challenge
The core question driving this research, a challenge that has perplexed immunologists for years, is simple: why do T-cells lose their ability to fight cancer? While numerous factors have been investigated - genetics, epigenetics, metabolic changes – a crucial piece of the puzzle remained elusive. Researchers at OSUCCC – James have now pinpointed a critical vulnerability within exhausted T-cells: an overwhelming accumulation of misfolded proteins.
Introducing TexPSR: A Novel Stress Pathway in T-Cell Exhaustion
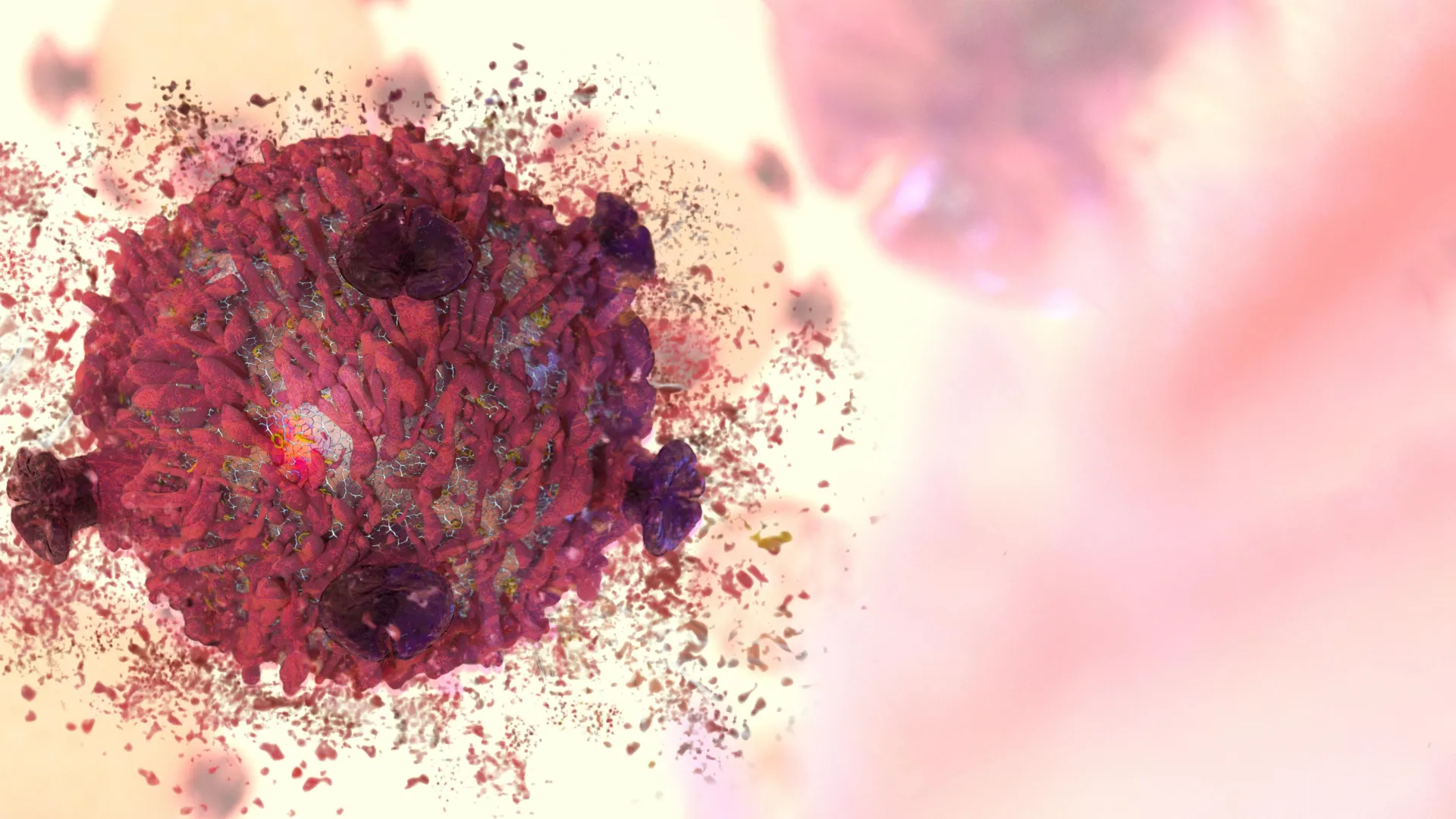
This accumulation isn’t a simple slowdown in protein production; it’s a paradoxical overdrive.The study reveals a unique stress pathway, termed TexPSR (proteotoxic stress response in T-cell exhaustion), where exhausted T-cells ramp up protein synthesis despite being unable to properly fold and process these proteins. This leads to a hazardous buildup of misfolded proteins, forming stress granules and toxic aggregates – a process disturbingly similar to the amyloid plaque formation observed in neurodegenerative diseases like Alzheimer’s.
This “proteotoxic shock,” as described by Nature Reviews Immunology, effectively poisons the T-cells, crippling their ability to mount an effective anti-tumor response. Rather of deploying functional immune weaponry, exhausted T-cells are caught in a destructive cycle of creating and destroying their own tools.
Reversing Exhaustion: Blocking TexPSR Restores T-Cell Function
The implications of this discovery are profound. In preclinical models, blocking key drivers of TexPSR resulted in a remarkable recovery of T-cell function. Critically, this restoration translated directly into considerably enhanced efficacy of cancer immunotherapy.
“T-cell exhaustion is the biggest roadblock to cancer immunotherapy,” explains dr. Zihai Li, MD, PhD, senior author of the study and founding Director of the pelotonia Institute for Immuno-oncology (PIIO) at the OSUCCC – James. “Our study results present a surprising and exciting answer to this fundamental problem and could be critical to improving future scientific advances in the field of engineered cancer drug therapies to harness the immune system.”
Dr. Li, a leading expert who has dedicated over three decades to studying the link between protein folding and immunity, emphasizes the novelty of this approach.”Researchers worldwide are tackling T-cell exhaustion thru studying genetics, epigenetics, metabolism and others, but the role of protein quality control has been largely overlooked — until now.”
Clinical Relevance: TexPSR as a Biomarker and Therapeutic Target
The research isn’t limited to laboratory findings.The OSUCCC – James team discovered a strong correlation between high levels of TexPSR in T-cells from cancer patients and poorer responses to immunotherapy.This suggests that TexPSR levels could serve as a valuable biomarker to predict treatment success and,crucially,that targeting this pathway could be a new strategy to enhance cancer treatment in the clinic.
The mechanism’s broad relevance is further underscored by its validation across multiple cancer types, including lung, bladder, liver cancer, and leukemia. This suggests a universal vulnerability in exhausted T-cells, regardless of the specific cancer being fought. The team’s findings are published in the latest issue of Nature.
The Future of Immunotherapy: A Paradigm Shift in Understanding
This research represents a paradigm shift in our understanding of T-cell exhaustion and opens up exciting new avenues for cancer immunotherapy. By focusing on the fundamental process of protein quality control within immune cells, scientists are poised to develop innovative therapies that can revitalize the immune system and unlock the full potential of cancer treatment.
Evergreen Section: The Importance of Protein Homeostasis in Immune Function
The discovery of TexPSR highlights a fundamental principle in biology: the critical importance of protein homeostasis. Maintaining the correct folding, modification, and degradation of proteins is essential for cellular function, and disruptions in this process are implicated in a wide range of diseases, from neurodegenerative disorders to cancer.The immune system, with its complex production of antibodies and signaling molecules, is notably sensitive to disruptions in protein homeostasis. Understanding and targeting these vulnerabilities represents a promising new frontier in therapeutic advancement, extending far beyond cancer immunotherapy to potentially address autoimmune diseases and chronic
![California High Schools That Produce the Most NFL Players [Year] – Updated Rankings California High Schools That Produce the Most NFL Players [Year] – Updated Rankings](https://i0.wp.com/superwestsports.com/wp-content/uploads/2025/10/Tetairoa-McMillan.jpg?resize=150%2C150&ssl=1)








