Yot Teerawattananon
2026-01-21 00:00:00
ISN–Global Kidney Health Atlas: A Report by the International Society of Nephrology: An Assessment of Global Kidney Health Care Status Focusing on Capacity, Availability, Accessibility, Affordability and Outcomes of Kidney Disease (International Society of Nephrology, 2023); https://www.theisn.org/initiatives/global-kidney-health-atlas/
Irish, G. L. et al. Breakthrough discoveries. ISN https://www.theisn.org/about-isn/history/breakthrough-discoveries/#breakthrough-aug (2020).
Liyanage, T. et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 385, 1975–1982 (2015).
Kalyesubula, R. et al. The future of kidney care in low- and middle-income countries: challenges, triumphs, and opportunities. Kidney360 5, 1047–1061 (2024).
Wainstein, M. et al. International Society of Nephrology Global Kidney Health Atlas: structures, organization, and services for the management of kidney failure in Latin America. Kidney Int. Suppl. (2011) 11, e35–e46 (2021).
Chung, R. et al. Economic evaluations in kidney transplantation: frequency, characteristics, and quality-a systematic review. Transplantation 97, 1027–1033 (2014).
Senanayake, S. et al. Cost-utility analysis in chronic kidney disease patients undergoing kidney transplant; what pays? A systematic review. Cost. Eff. Resour. Alloc. 18, 18 (2020).
Wyld, M. et al. A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments. PLoS Med. 9, e1001307 (2012).
Yang, F. et al. The cost-effectiveness of kidney replacement therapy modalities: a systematic review of full economic evaluations. Appl. Health Econ. Health Policy 19, 163–180 (2021).
Fu, R. et al. Cost-effectiveness of deceased-donor renal transplant versus dialysis to treat end-stage renal disease: a systematic review. Transpl. Direct 6, e522 (2020).
NHS Blood and Transplant reveals nearly 49,000 people in the UK have had to wait for a transplant in the last decade. NHS Blood and Transplant https://www.organdonation.nhs.uk/get-involved/news/nearly-49-000-people-in-uk-have-had-to-wait-for-a-transplant-in-the-last-decade/ (2015).
Improving dialysis for patients and health systems in community and home care. MedTech Europe https://www.medtecheurope.org/resource-library/improving-dialysis-for-patients-and-health-systems-in-community-and-home-care/ (2015).
Yeung, E. et al. Current status of health systems financing and oversight for end-stage kidney disease care: a cross-sectional global survey. BMJ Open 11, e047245 (2021).
Tang, S. C. W. et al. Dialysis care and dialysis funding in Asia. Am. J. Kidney Dis. 75, 772–781 (2020).
Teerawattananon, Y. et al. To include or not include: renal dialysis policy in the era of universal health coverage. Brit. Med. J. 368, m82 (2020).
Teerawattananon, Y. et al. Dispelling the myths of providing dialysis in low- and middle-income countries. Nat. Rev. Nephrol. 17, 11–12 (2021).
Sangthawan, P. et al. The hidden financial catastrophe of chronic kidney disease under universal coverage and Thai “Peritoneal Dialysis First Policy”. Front. Public Health 10, 965808 (2022).
Chuengsaman, P. et al. PD first policy: Thailand’s response to the challenge of meeting the needs of patients with end-stage renal disease. Semin. Nephrol. 37, 287–295 (2017).
Kanjanabuch, T. et al. Implementation of PDOPPS in a middle-income country: early lessons from Thailand. Perit. Dial. Int. 42, 83–91 (2022).
Dhanakijcharoen, P., Sirivongs, D., Aruyapitipan, S., Chuengsaman, P. & Lumpaopong, A. The “PD first” policy in Thailand: three-years experiences (2008-2011). J. Med Assoc. Thai 94, S153–S161 (2011).
Bayani, D. B. S. et al. Filtering for the best policy: an economic evaluation of policy options for kidney replacement coverage in the Philippines. Nephrol. (Carlton) 26, 170–177 (2021).
Empowering Ghana’s path to sustainable healthcare: HITAP’s HTA capacity building workshop in Ghana. Health Intervention and Technology Assessment Program https://www.hitap.net/en/news/ghana-hta-capacity-building/ (2023).
Afiatin et al. Economic evaluation of policy options for dialysis in end-stage renal disease patients under the universal health coverage in Indonesia. PLoS ONE 12, e0177436 (2017).
Liu, F. X. et al. A global overview of the impact of peritoneal dialysis first or favored policies: an opinion. Perit. Dial. Int. 35, 406–420 (2015).
Kidney Friends Club complains that the Gold Card does not provide equal rights for dialysis. MGR Online https://mgronline.com/qol/detail/9540000061292 (2011).
PD first policy “violation of rights” or “patients have access to treatment”. MGR Online https://mgronline.com/qol/detail/9590000095013 (2016).
New HD cost reimbursement policy will ease heavy burden on kidney patients. National Health Security Office https://eng.nhso.go.th/view/1/DescriptionNews/New-HD-cost-reimbursement-policy-will-ease-heavy-burden-on-kidney-patients/416/EN-US#:~:text=The%20decision%20by%20the%20National,all%20kidney%20patients%2C%20he%20said (2022).
The World Bank in Thailand. World Bank https://www.worldbank.org/en/country/thailand/overview (2024).
Thailand now an upper middle income economy. World Bank https://www.worldbank.org/en/news/press-release/2011/08/02/thailand-now-upper-middle-income-economy (2011).
GDP per Capita (Current US$) – Thailand (World Bank Group, accessed 10 November 2025); https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=TH
Tangcharoensathien, V. et al. Promoting universal financial protection: how the Thai universal coverage scheme was designed to ensure equity. Health Res. Policy Syst. 11, 25 (2013).
Tangcharoensathien, V. et al. The political economy of UHC reform in Thailand: lessons for low- and middle-income countries. Health Syst. Reform 5, 195–208 (2019).
NHSO Annual Report Fiscal Year 2022 (NHSO, 2022); https://eng.nhso.go.th/view/1/Annual_Reports/EN-US
Ingsathit, A. et al. Prevalence and risk factors of chronic kidney disease in the Thai adult population: Thai SEEK study. Nephrol. Dial. Transpl. 25, 1567–1575 (2009).
Rajatanavin, N. et al. Effective coverage of diabetes and hypertension: an analysis of Thailand’s national insurance database 2016-2019. BMJ Open 12, e066289 (2022).
Sakboonyarat, B. et al. Characteristics and clinical outcomes of people with hypertension receiving continuous care in Thailand: a cross-sectional study. Lancet Reg. Health Southeast Asia 21, 100319 (2024).
Tiptaradol, S. et al. Prevalence, awareness, treatment and control of coexistence of diabetes and hypertension in thai population. Int. J. Hypertens. 2012, 386453 (2012).
Ministry of Public Health of Thailand et al. Prevention and Control of Noncommunicable Diseases in Thailand: The Case for Investment (UNDP and WHO, 2021); https://www.undp.org/sites/g/files/zskgke326/files/migration/th/UNDP_TH_WHO_THAILAND_NCD-IC-REPORT_v06_231121.pdf
Praditpornsilpa, K. et al. in Nephrology Worldwide (eds Moura-Neto, J. A. et al.) Ch. 31 (Springer, 2021).
Paffett, M. et al. Economic evaluation of an integrated care program compared to conventional care for patients with chronic kidney disease in rural communities of Thailand. Kidney Int. Rep. 9, 2546–2558 (2024).
Jiamjariyapon, T. et al. Effectiveness of integrated care on delaying progression of stage 3-4 chronic kidney disease in rural communities of Thailand (ESCORT study): a cluster randomized controlled trial. BMC Nephrol. 18, 83 (2017).
Thanachayanont, T. et al. Effectiveness of integrated care on delaying chronic kidney disease progression in rural communities of Thailand (ESCORT-2) trials. Nephrol. (Carlton) 26, 333–340 (2021).
Davison, S. N. et al. Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney Int. 88, 447–459 (2015).
Scaling Up Antiretroviral Treatment: Lessons Learnt from Thailand – Report of an External Evaluation (World Health Organization Regional Office for South-East Asia, 2004); https://www.aidsdatahub.org/sites/default/files/resource/scaling-antiretroviral-treatment-lessons-learnt-thailand.pdf
Tangcharoensathien, V. et al. Universal Access to Renal Replacement Therapy in Thailand: A Policy Analysis (HSRI, 2005); https://kb.hsri.or.th/dspace/handle/11228/1522?show=full
Sirivongs, D. et al. Fact About PD First Policy in Thailand (PD Technology and Training Center, Srinagarind Hospital, Khon Kaen University, 2011).
Changsirikulchai, S. et al. Survival analysis and associated factors in Thai patients on peritoneal dialysis under the PD-first policy. Perit. Dial. Int. 38, 172–178 (2018).
Perl, J. et al. Peritoneal dialysis-related infection rates and outcomes: results from the Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS). Am. J. Kidney Dis. 76, 42–53 (2020).
Six organizations announced the success of “10 years of peritoneal dialysis policy” to help patients access treatment. The Coverage https://www.thecoverage.info/news/content/259 (2018).
Tangcharoensathien, V. et al. Health systems development in Thailand: a solid platform for successful implementation of universal health coverage. Lancet 391, 1205–1223 (2018).
Teerawattananon, Y. et al. Fifteen lessons from fifteen years of the health intervention and technology assessment program in Thailand. Health Syst. Reform 9, 2330974 (2023).
Satirapoj, B. et al. Thailand Renal Replacement Therapy Registry 2023 annual data report: dialysis center providers in Thailand. J. Nephrol. Soc. Thai 31, 1–10 (2025).
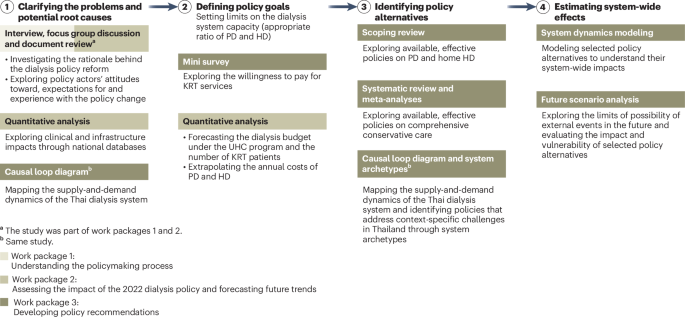
Botwright, S. et al. Understanding healthcare demand and supply through causal loop diagrams and system archetypes: policy implications for kidney replacement therapy in Thailand. BMC Med. 23, 231 (2025).
Registration procedures for specialized hemodialysis (HD) referral service units, 2021 [in Thai]. National Health Security Office https://www.nhso.go.th/th/communicate-th/new/2024-10-30-15-39-50/11318-hd-2564 (2021).
Wolstenholme, E. F. Towards the definition and use of a core set of archetypal structures in system dynamics. Syst. Dyn. Rev. 19, 7–26 (2003).
Chawla, N. et al. Policy strategies to enhance uptake of conservative kidney management in advanced chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol. 26, 388 (2025).
Yongphiphatwong, N. et al. The way home: a scoping review of public health interventions to increase the utilization of home dialysis in chronic kidney disease patients. BMC Nephrol. 26, 169 (2025).
Liu, A. Y. L. et al. Nephrologists-led intervention increases utilisation of peritoneal dialysis in Singapore. Ann. Acad. Med. Singap. 50, 919–921 (2021).
Asif, A. et al. Does catheter insertion by nephrologists improve peritoneal dialysis utilization? A multicenter analysis. Semin. Dial. 18, 157–160 (2005).
Alderson, P. Critical Realism for Health and Illness Research: A Practical Introduction (Policy Press Scholarship Online, 2021).
Schloemer, T. et al. Criteria for evaluating transferability of health interventions: a systematic review and thematic synthesis. Implement. Sci. 13, 88 (2018).
Rutter, H. et al. The need for a complex systems model of evidence for public health. Lancet 390, 2602–2604 (2017).
Botwright, S. et al. Balancing patient choice and health system capacity: a system dynamics model of dialysis in Thailand. BMC Med. 23, 646 (2025).
Maier, H. R. et al. An uncertain future, deep uncertainty, scenarios, robustness and adaptation: how do they fit together?. Environ. Model. Softw. 81, 154–164 (2016).
Richardson, G. P. Reflections on the foundations of system dynamics. Syst. Dyn. Rev. 27, 219–243 (2011).
Gerhold, L. et al. (eds) Standards of Futures Research (Springer, 2022).
Walker, W. E. et al. Encyclopedia of Operations Research and Management Science (Springer, 2013).
Botwright, S. et al. A case study integrating scenario thinking with dialysis policymaking in Thailand. Comm. Med. https://doi.org/10.1038/s43856-025-01299-3 (2025).
Glickman, A. et al. Conflicts of interest in dialysis: a barrier to policy reforms. Semin. Dial. 33, 83–89 (2020).
Kanter, G. et al. Hidden physician financial conflicts of interest in dialysis: nephrologists’ ownership of dialysis facilities doesn’t affect outcomes, but why is it so secret? Penn LDI https://ldi.upenn.edu/our-work/research-updates/hidden-physician-financial-conflicts-of-interest-in-dialysis/ (2022).
Williams, M. E. et al. The involuntarily discharged dialysis patient: conflict (of interest) with providers. Adv. Chronic Kidney Dis. 12, 107–112 (2005).
Lin, E. et al. Association between nephrologist ownership of dialysis facilities and clinical outcomes. JAMA Intern. Med. 182, 1267–1276 (2022).
ISN Framework for Developing Dialysis Programs in Low-resource Settings (ISN, 2021); https://www.theisn.org/wp-content/uploads/2021/03/ISN-Framework-Dialysis-Report-HIRES.pdf
Shiell, A. et al. Complex interventions or complex systems? Implications for health economic evaluation. Brit. Med. J. 336, 1281–1283 (2008).
Wright, M. A need for systems thinking and the appliance of (complexity) science in healthcare. Future Health J. 11, 100185 (2024).
Glicken, J. Getting stakeholder participation ‘right’: a discussion of participatory processes and possible pitfalls. Environ. Sci. Policy 3, 305–310 (2000).
van Ast, J. A. et al. Participation in European water policy. Phys. Chem. Earth 28, 555–562 (2003).
Cassidy, R. et al. Mathematical modelling for health systems research: a systematic review of system dynamics and agent-based models. BMC Health Serv. Res. 19, 845 (2019).
Davahli, M. R. et al. A system dynamics simulation applied to healthcare: a systematic review. Int J. Environ. Res. Public Health 17, 5741 (2020).
Nguyen, L.-K.-N. et al. Implementation of systems thinking in public policy: a systematic review. Systems 11, 64 (2023).
Systems Thinking for Health Systems Strengthening (WHO, 2009); https://evidence-impact.org/tools/identify-high-priority-issue/Systems-thinking-for-health-systems-strengthening
Wasi, P. Triangle that Moves the Mountain and Health Systems Reform Movement in Thailand (HSRI, 2000).
Labrique, A. B. et al. Best practices in scaling digital health in low and middle income countries. Glob. Health 14, 103 (2018).
Tsoukas, H. The tyranny of light: the temptations and the paradoxes of the information society. Futures 29, 827–843 (1997).
Order of the National Health Security Office No. 204/2567 Subject: Appointing a Working Group to Develop Dialysis Policies Under the National Health Insurance System (NHSO, 2024).
Teerawattananon, Y. et al. Economic evaluation of palliative management versus peritoneal dialysis and hemodialysis for end-stage renal disease: evidence for coverage decisions in Thailand. Value Health 10, 61–72 (2007).