Understanding IVF Outcomes in Different Polycystic Ovary Syndrome (PCOS) Subtypes
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder affecting many women of reproductive age. Though, it’s becoming increasingly clear that PCOS isn’t a single condition, but rather a spectrum of subtypes. This understanding is crucial, as IVF outcomes can vary substantially depending on which type of PCOS a woman has. This article delves into a recent study examining these differences, providing you with a comprehensive overview of teh findings and what they mean for your fertility journey.
Why PCOS Subtyping matters for IVF
Traditionally, PCOS diagnosis focused on the Rotterdam criteria – irregular periods, polycystic ovaries, and signs of hyperandrogenism (excess androgens). But this broad definition doesn’t account for the diverse ways PCOS manifests. Recent research, including the study we’ll discuss, highlights the importance of identifying specific subtypes to personalize treatment and improve IVF success rates.
This research, published in Front. Pharmacol. (J. et al. Chinese guideline for lipid management. Front. Pharmacol. 14, 1190934 (2023)), analyzed data from a large cohort of women undergoing IVF, comparing outcomes across different PCOS subtypes and a control group. Let’s break down the study’s methodology and key findings.
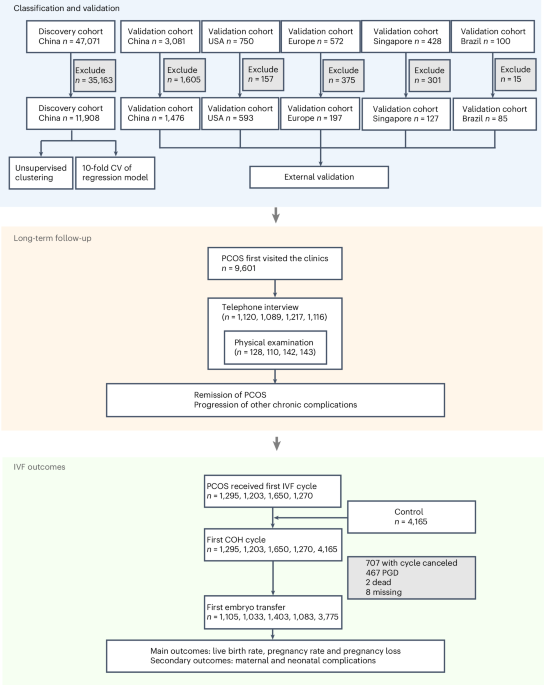
Study Design: How the Research Was Conducted
Researchers analyzed data from 5,418 participants in a finding cohort undergoing IVF. To provide a meaningful comparison, they included a control group of women undergoing IVF for other reasons, specifically:
* fallopian tube issues: Infertility due to blocked or adhered fallopian tubes, without any PCOS characteristics.
* Male factor infertility: Infertility stemming from low sperm count, poor sperm motility, or abnormal sperm morphology in their partner.
The study focused on several key outcomes:
* Primary Outcomes: Live birth rate, pregnancy rate, and pregnancy loss.
* Secondary Outcomes: Maternal and neonatal complications, including preterm delivery, premature rupture of membranes, and birth weight (small for Gestational Age - SGA, and Large for Gestational Age – LGA).
Defining Key IVF outcomes
To ensure clarity, the researchers used specific definitions for vital terms:
* Conception: confirmed by a serum human chorionic gonadotropin (hCG) level of ≥10 mIU/ml.
* Clinical Pregnancy: Visualized as a gestational sac within the uterus.
* First Trimester Pregnancy Loss: Loss before the end of the 11th week of gestation (miscarriage or stillbirth).
* Second Trimester Pregnancy Loss: loss between the 12th and 27th week of gestation (miscarriage or stillbirth due to fetal abnormalities, maternal factors, or preterm birth).
* Preterm Delivery: Live birth between the 28th and 36th week of gestation (including induced preterm births).
* Premature Rupture of Membranes: Membrane rupture after the 28th week, frequently enough linked to spontaneous preterm delivery.
* SGA & LGA: Determined using Chinese birth weight reference percentiles adjusted for sex and gestational age (Dai, L. et al. PLoS ONE 9, e104779 (2014)). SGA is defined as below the 10th percentile, and LGA as above the 90th percentile.
Statistical Analysis: Ensuring Reliable Results
The researchers employed robust statistical methods to analyze the data, using both SPSS v.26 and R v.4.0.3.Here’s a breakdown:
* Normality testing: Shapiro-Wilk tests were used to determine if data followed a normal distribution.
* Continuous Data Comparison: Student’s t-test or analysis of variance (ANOVA) were used, with logarithmic conversion for non-normal data. Post-hoc tests (Bonferroni or Dunnett T3) were used for comparisons between subtypes.
* Categorical Data Comparison: Chi-squared or Fisher’s exact tests were used.
* Odds Ratios (ORs): Logistic regression was used to calculate ORs for each PCOS subtype compared to the control group.This analysis accounted for potential confounding factors:
* Model 1: Age and ovarian stimulation methods.
* model 2: Age



![HCA Integration: New Hampshire Hospital CEO Strategy | [Hospital Name] HCA Integration: New Hampshire Hospital CEO Strategy | [Hospital Name]](https://i0.wp.com/www.beckershospitalreview.com/wp-content/uploads/sites/9/2025/03/BeckersHospitalReview.jpg?resize=330%2C220&ssl=1)




