Okay, here’s a comprehensive, authoritative article based on the provided text, designed to meet your E-E-A-T, SEO, and engagement goals. It’s crafted to sound like it’s written by a seasoned expert in the field, while remaining accessible to a broad audience. I’ve focused on clarity, depth, and a conversational tone. I’ve also incorporated elements to aid indexing and engagement.
Please read the ”Critically important Considerations” section at the end before publishing.
Navigating the Changing Landscape of Family Planning access in the US
Access to comprehensive family planning services is a cornerstone of public health, empowering individuals to make informed decisions about their reproductive lives. Though, this access is increasingly under pressure, facing a complex web of policy changes, funding shifts, and evolving regulations. This article provides an in-depth look at the current state of family planning access in the United States, focusing on the key providers and the challenges they face. We’ll break down the impact of recent changes and what they mean for individuals seeking care.
The Core Providers: A Safety net Under Strain
The US family planning safety net relies on a diverse network of providers, each with a unique role and funding structure. Let’s examine the key players:
Title X Clinics: Administered by the Department of Health and Human Services (HHS), title X is the only federal program dedicated solely to family planning. These clinics provide a range of essential services – contraception, STI screening and treatment, pregnancy testing, and basic reproductive health care – primarily to low-income and uninsured individuals. However, recent policy shifts have substantially impacted Title X.
Section 330 Federally qualified Health Centers (FQHCs): FQHCs are community-based health centers that receive federal funding to provide comprehensive primary care services,including family planning,in underserved areas. They are legally obligated to serve all patients nonetheless of their ability to pay or immigration status. FQHCs are a vital access point, particularly for vulnerable populations.
Planned Parenthood: A nationally recognized provider, Planned Parenthood delivers a wide spectrum of reproductive health services, including contraception, abortion care, and cancer screenings. They serve millions of patients annually and are a critical resource, especially in areas with limited access to other providers.
Indian health Service (IHS) & Tribal Clinics: The IHS, an agency within HHS, provides healthcare to approximately 2.8 million American Indian and Alaska Native (AIAN) individuals. Services are generally free at the point of care for eligible members of federally recognized Tribes. While federal regulations mandate coverage of family planning, the availability of specific contraceptive methods can vary.
Rural Health Clinics (rhcs): Located in designated health professional shortage areas, RHCs provide primary and preventive care to rural communities. They receive enhanced reimbursement rates for Medicaid and Medicare patients and can offer contraceptive services, though the extent varies.
recent Policy Changes & Their Impact
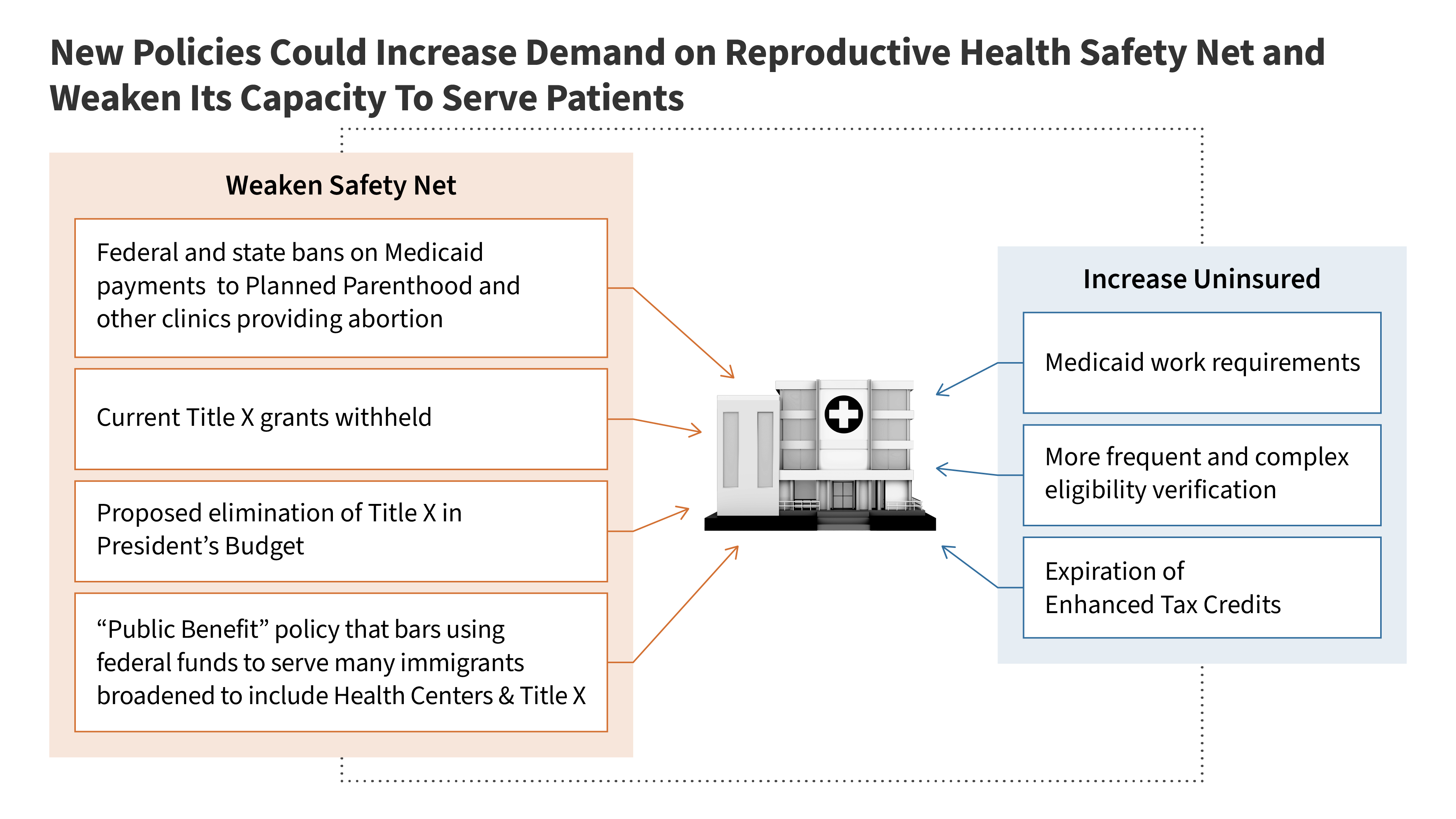
The landscape of family planning access has been dramatically reshaped in recent years. Here’s a breakdown of the most significant changes:
The “Protect Life Rule” (and its Rescission): The Trump Management implemented a rule prohibiting Title X funds from being used at clinics that provide abortion referrals or services.This effectively defunded Planned Parenthood and many other Title X providers. The Biden Administration rescinded this rule in 2021, restoring funding to these clinics, but the impact of the years-long disruption is still being felt.
Restrictions on “Public Benefits” & Immigration Status: A recent policy change bars individuals deemed to be receiving ”public benefits” - including those accessing Title X and Section 330 funds - if they are undocumented. This creates a chilling effect, as clinics are now required to verify immigration status, possibly deterring eligible individuals from seeking care. This policy directly conflicts with the legal obligation of FQHCs to serve all patients, regardless of immigration status, creating significant legal and ethical challenges.
Budget Reconciliation & Medicaid Cuts: The 2025 Budget Reconciliation Law is projected to increase the number of uninsured americans, placing additional strain on safety net providers like IHS and FQHCs. These facilities rely heavily on Medicaid reimbursements (around 70% for IHS) and will face resource constraints as more patients become uninsured.
* Potential Pressure on Rural Health Clinics: The defunding of Planned Parenthood in some areas could increase demand for reproductive health services at Rural Health