Aldo Alberto Conti
2026-01-16 00:00:00
Cortese, S. et al. Incidence, prevalence, and global burden of ADHD from 1990 to 2019 across 204 countries: data, with critical re-analysis, from the Global Burden of Disease study. Mol. Psychiatry 28, 4823–4830 (2023).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) (American Psychiatric Association Publishing, 2022).
Pievsky, M. A. & McGrath, R. E. The neurocognitive profile of attention-deficit/hyperactivity disorder: a review of meta-analyses. Arch. Clin. Neuropsychol. 33, 143–157 (2018).
Huang-Pollock, C. L., Karalunas, S. L., Tam, H. & Moore, A. N. Evaluating vigilance deficits in ADHD: a meta-analysis of CPT performance. J. Abnorm. Psychol. 121, 360–371 (2012).
Rubia, K. Cognitive neuroscience of attention deficit hyperactivity disorder (ADHD) and its clinical translation. Front. Hum. Neurosci. 12, 100 (2018).
Faraone, S. V. et al. Attention-deficit/hyperactivity disorder. Nat. Rev. Dis. Primers 10, 11 (2024).
Cortese, S. et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry 5, 727–738 (2018).
Brikell, I. et al. ADHD medication discontinuation and persistence across the lifespan: a retrospective observational study using population-based databases. Lancet Psychiatry 11, 16–26 (2024).
Swanson, J. M. Risk of bias and quality of evidence for treatment of ADHD with stimulant medication. Clin. Pharmacol. Ther. 104, 638–643 (2018).
Fusar-Poli, P., Rubia, K., Rossi, G., Sartori, G. & Balottin, U. Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis. Am. J. Psychiatry 169, 264–272 (2012).
Isfandnia, F., El Masri, S., Radua, J. & Rubia, K. The effects of chronic administration of stimulant and non-stimulant medications on executive functions in ADHD: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 162, 105703 (2024).
Schatz, N. K. et al. Systematic review of patients’ and parents’ preferences for ADHD treatment options and processes of care. Patient 8, 483–497 (2015).
Rubia, K., Westwood, S., Aggensteiner, P. M. & Brandeis, D. Neurotherapeutics for attention deficit/hyperactivity disorder (ADHD): a review. Cells 10, 2156 (2021).
Powell, K. et al. Trigeminal nerve stimulation: a current state-of-the-art review. Bioelectron. Med. 9, 30 (2023).
Aston-Jones, G. & Waterhouse, B. Locus coeruleus: from global projection system to adaptive regulation of behavior. Brain Res. 1645, 75–78 (2016).
Mercante, B., Enrico, P. & Deriu, F. Cognitive functions following trigeminal neuromodulation. Biomedicines 11, 2392 (2023).
Bellato, A., Arora, I., Hollis, C. & Groom, M. J. Is autonomic nervous system function atypical in attention deficit hyperactivity disorder (ADHD)? A systematic review of the evidence. Neurosci. Biobehav. Rev. 108, 182–206 (2020).
Faraone, S. V. & Radonjić, N. V. Neurobiology of attention deficit hyperactivity disorder. in Tasman’s Psychiatry 1–28 (Springer, 2023); https://doi.org/10.1007/978-3-030-42825-9_33-1
Westwood, S. J. et al. Clinical and cognitive effects of external trigeminal nerve stimulation (eTNS) in neurological and psychiatric disorders: a systematic review and meta-analysis. Mol. Psychiatry 28, 4025–4043 (2023).
McGough, J. J. et al. Double-blind, sham-controlled, pilot study of trigeminal nerve stimulation for attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 58, 403–411 (2019).
DuPaul, G.J., Power, T.J., Anastopoulos, A.D. & Reid, R. ADHD Rating Scale-5 for Children and Adolescents: Checklists, Norms, and Clinical Interpretation (Guilford Press, 2016).
Lukito, S. et al. Comparative meta-analyses of brain structural and functional abnormalities during cognitive control in attention-deficit/hyperactivity disorder and autism spectrum disorder. Psychol. Med. 50, 894–919 (2020).
Hart, H., Radua, J., Mataix-Cols, D. & Rubia, K. Meta-analysis of fMRI studies of timing in attention-deficit hyperactivity disorder (ADHD). Neurosci. Biobehav. Rev. 36, 2248–2256 (2012).
Hart, H., Radua, J., Nakao, T., Mataix-Cols, D. & Rubia, K. Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects. JAMA Psychiatry 70, 185–198 (2013).
Norman, L. J. et al. Structural and functional brain abnormalities in attention-deficit/hyperactivity disorder and obsessive-compulsive disorder: a comparative meta-analysis. JAMA Psychiatry 73, 815–825 (2016).
McGough, J. J. et al. An eight-week, open-trial, pilot feasibility study of trigeminal nerve stimulation in youth with attention-deficit/hyperactivity disorder. Brain Stimul. 8, 299–304 (2015).
Bozhilova, N. S., Michelini, G., Kuntsi, J. & Asherson, P. Mind wandering perspective on attention-deficit/hyperactivity disorder. Neurosci. Biobehav. Rev. 92, 464–476 (2018).
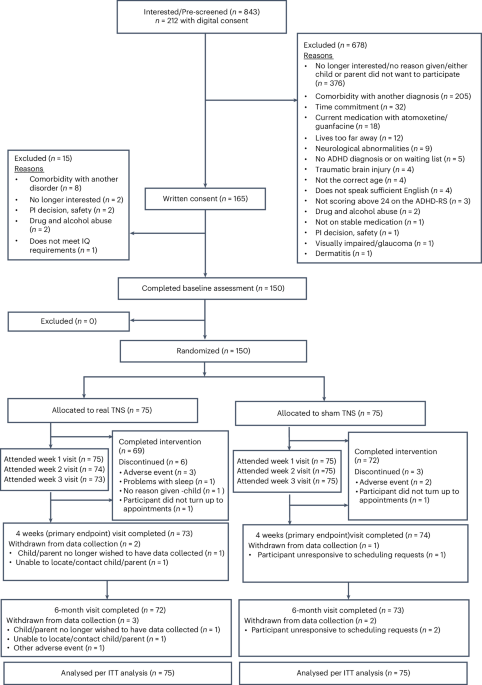
Rubia, K. et al. The efficacy of real versus sham external trigeminal nerve stimulation (eTNS) in youth with attention-deficit/hyperactivity disorder (ADHD) over 4 weeks: a protocol for a multi-centre, double-blind, randomized, parallel-group, phase IIb study (ATTENS). BMC Psychiatry 24, 326 (2024).
Thibault, R. T. & Raz, A. The psychology of neurofeedback: clinical intervention even if applied placebo. Am. Psychol. 72, 679–688 (2017).
Huneke, N. T. M. et al. Placebo effects in randomized trials of pharmacological and neurostimulation interventions for mental disorders: an umbrella review. Mol. Psychiatry 29, 3915–3925 (2024).
Rief, W. & Wilhelm, M. Nocebo and placebo effects and their implications in psychotherapy. Psychother. Psychosom. 93, 298–303 (2024).
Thibault, R. T., Veissière, S., Olson, J. A. & Raz, A. Treating ADHD with suggestion: neurofeedback and placebo therapeutics. J. Atten. Disord. 22, 707−711 (2018).
Faraone, S. V. et al. Placebo and nocebo responses in randomised, controlled trials of medications for ADHD: a systematic review and meta-analysis. Mol. Psychiatry 27, 212–219 (2022).
Christakou, A. et al. Disorder-specific functional abnormalities during sustained attention in youth with attention deficit hyperactivity disorder (ADHD) and with autism. Mol. Psychiatry 18, 236–244 (2013).
Norman, L. J., Sudre, G., Price, J., Shastri, G. G. & Shaw, P. Evidence from ‘big data’ for the default-mode hypothesis of ADHD: a mega-analysis of multiple large samples. Neuropsychopharmacology 48, 281–289 (2023).
Dekkers, T. J. et al. Does mind-wandering explain ADHD-related impairment in adolescents? Child Psychiatry Hum. Dev. 56, 346–357 (2025).
Lanier, J., Noyes, E. & Biederman, J. Mind wandering (internal distractibility) in ADHD: a literature review. J. Atten. Disord. 25, 885–890 (2021).
Frick, M. A., Asherson, P. & Brocki, K. C. Mind-wandering in children with and without ADHD. Br. J. Clin. Psychol. 59, 208–223 (2020).
Mowlem, F. D. et al. Validation of the mind excessively wandering scale and the relationship of mind wandering to impairment in adult ADHD. J. Atten. Disord. 23, 624–634 (2019).
Loo, S. K. et al. Trigeminal nerve stimulation for attention-deficit/hyperactivity disorder: cognitive and electroencephalographic predictors of treatment response. J. Am. Acad. Child Adolesc. Psychiatry 60, 856–864 (2021).
Anastopoulos, A. D. et al. Impact of child and informant gender on parent and teacher ratings of attention-deficit/hyperactivity disorder. Psychol. Assess. 30, 1390–1394 (2018).
Vazquez, A. L., Sibley, M. H. & Campez, M. Measuring impairment when diagnosing adolescent ADHD: differentiating problems due to ADHD versus other sources. Psychiatry Res. 264, 407–411 (2018).
Stirratt, M. J. et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl. Behav. Med. 5, 470–482 (2015).
Ostinelli, E. G. et al. Comparative efficacy and acceptability of pharmacological, psychological, and neurostimulatory interventions for ADHD in adults: a systematic review and component network meta-analysis. Lancet Psychiatry 12, 32–43 (2025).
Rubia, K. Neurotherapeutics for ADHD: do they work? Psych. J. 11, 419–427 (2022).
Schertz, M. et al. Transcranial direct current stimulation (tDCS) in children with ADHD: a randomized, sham-controlled pilot study. J. Psychiatr. Res. 155, 302–312 (2022).
Westwood, S. J. et al. Transcranial direct current stimulation (tDCS) combined with cognitive training in adolescent boys with ADHD: a double-blind, randomised, sham-controlled trial. Psychol. Med. 53, 497–512 (2023).
Westwood, S. J., Radua, J. & Rubia, K. Noninvasive brain stimulation in children and adults with attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. J. Psychiatry Neurosci. 46, E14–E33 (2021).
Schulz, K. F., Altman, D. G., Moher, D. & CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann. Intern. Med. 152, 726–732 (2010).
Kaufman, J. et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–988 (1997).
Wechsler, D. Wechsler Abbreviated Scale of Intelligence https://psycnet.apa.org/doi/10.1037/t15170-000 (American Psychological Association, 1999).
Cortese, S. Pharmacologic treatment of attention deficit–hyperactivity disorder. N. Engl. J. Med. 383, 1050–1056 (2020).
Rubia, K., Smith, A. & Taylor, E. Performance of children with attention deficit hyperactivity disorder (ADHD) on a test battery of impulsiveness. Child Neuropsychol. 13, 276–304 (2007).
DuPaul, G. J., Power, T. J., Anastopoulos, A. D. & Reid, R. ADHD Rating Scale-IV: School Checklist https://psycnet.apa.org/doi/10.1037/t00680-000 (American Psychological Association, 1998).
Conners, C. K. Conners, Third Edition (Conners 3) (Western Psychological Services, 2008).
Goodman, R. The Strengths and Difficulties Questionnaire: a research note. J. Child Psychol. Psychiatry 38, 581–586 (1997).
Stringaris, A. et al. The Affective Reactivity Index: a concise irritability scale for clinical and research settings. J. Child Psychol. Psychiatry 53, 1109–1117 (2012).
Chorpita, B. F., Yim, L., Moffitt, C., Umemoto, L. A. & Francis, S. E. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav. Res. Ther. 38, 835–855 (2000).
Posner, K. et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 168, 1266–1277 (2011).
Bruni, O. et al. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J. Sleep Res. 5, 251–261 (1996).
Lichstein, K. L., Riedel, B. W. & Richman, S. L. The Mackworth Clock Test: a computerized version. J. Psychol. 134, 153–161 (2000).
Li, G. et al. An introduction to multiplicity issues in clinical trials: the what, why, when and how. Int. J. Epidemiol. 46, 746–755 (2017).
Conti, A. A. et al. The efficacy of external trigeminal nerve stimulation (TNS) in youth with attention-deficit/hyperactivity disorder (ADHD): a multi-centre, double-blind, randomized, sham-controlled, parallel-group, phase IIb trial (ATTENS). figshare https://doi.org/10.6084/m9.figshare.29414744.v1 (2025).